If you received a Form 1095-B or Form 1095-C from the State of California and you have questions, you are in the right place.
Introduction
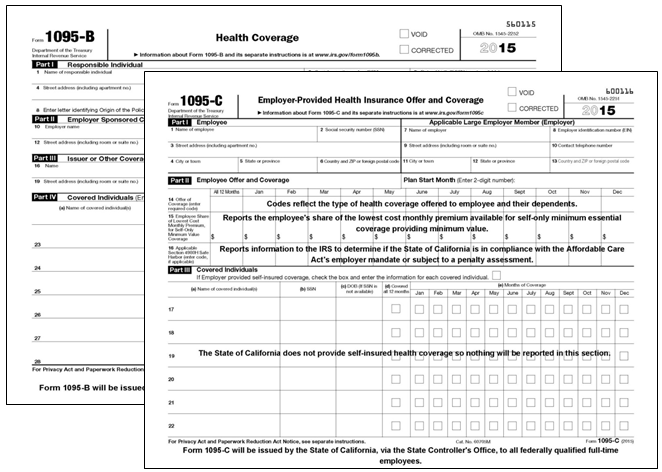
The Affordable Care Act (ACA) requires large employers to file annual reports with the Internal Revenue Service (IRS) and furnish a statement to full-time employees with information about the health coverage offered to the employee, their spouse and dependents, using IRS Form 1095-C. Health coverage providers are also required to file annual reports with the IRS and may provide a statement to individuals with information about those who had minimum essential coverage for at least one day during the preceding calendar year, using IRS Form 1095-B. The IRS Form 1095-B may also be provided upon request from the subscriber.
No later than 30 days after January 31, the State of California, via the State Controller's Office, will issue a Form 1095-C to its full-time employees with information about the health coverage offered, if any, to the employee, their spouse and dependents. The state's health coverage providers may also issue a Form 1095-B to employees who were enrolled in state-sponsored health coverage for at least one day during the preceding calendar year.
Below are answers to frequently asked questions about these forms.